Horizon Report
The state of cybersecurity in healthcare

As we enter 2025, the healthcare sector will be confronted with a rise in cyberattacks, strict legislative regulations, and the ongoing enhancement of AI, all while navigating financial pressures.
There are no “one-size-fits-all” answers to confronting these challenges. That is why collaboration is critical to safeguarding cybersecurity risks. By continuing to strengthen and expand our partnerships across the healthcare ecosystem — from payers to providers to technology companies to biotech — we enhance our resources and expertise. This is how we help you respond even more effectively to breaches, stay ahead of threats, and meet new regulatory requirements.
Fortified’s trusted team of industry experts, featured in this Horizon Report, actively engages year-round in cybersecurity discussions through roundtables, webinars, panels, and advisory committees. They are dedicated to gathering new insights and best practices, empowering us to problem-solve as a unified, collaborative community.
Let’s use these collaborative efforts to advance enhanced security, tailored solutions, and efficient compliance and risk management. Let’s strengthen staff training, perform continuous security assessments, and improve incident response, so all healthcare organizations can possess a resilient defense system to tackle emerging threats.
At Fortified Health Security, we are referred to as “Healthcare’s Cybersecurity Partner” because we know partnerships are the key to success. Looking ahead, we remain dedicated to continuing our collaboration with the entire healthcare industry and sharing our solutions to protect your data and patient lives.
Together, we can secure the future of healthcare and safeguard patient trust.
Warm regards,
Dan L. Dodson
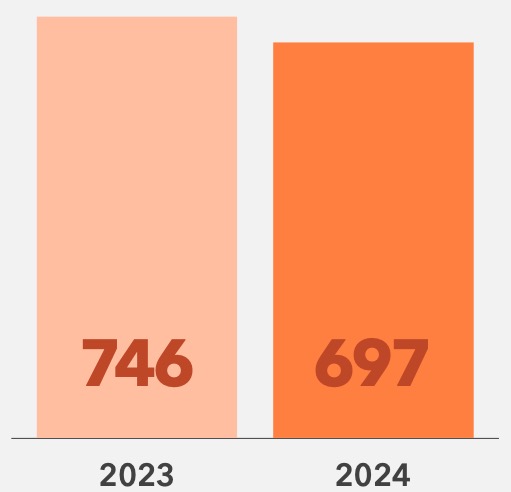
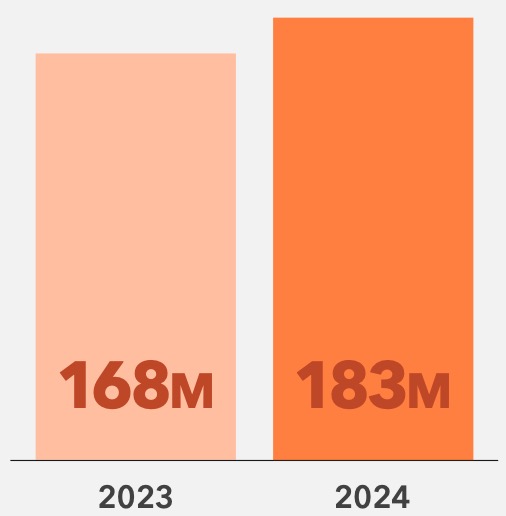
In 2024, while the number of cybersecurity breaches decreased 7% year over year, their impact grew significantly. In fact, more than 15 million additional patients were affected by breaches than in 2023.
Cybercriminals are becoming more sophisticated, exploiting new threat vectors such as third-party vendors, and employing advanced techniques. These attacks are no longer just about stealing data—they’re disrupting and even shutting down entire healthcare operations.
Mitigating these complex threats requires investment in cybersecurity personnel and defense systems. However, budget constraints and a growing talent gap make it increasingly challenging to safeguard patients and healthcare organizations.
There are actionable solutions outlined throughout the Horizon Report to address these complex threats. But to mitigate or remediate these threats we must start with a clear view and understanding of the data from the 2024 key breaches.
The following should serve as a wake-up call across the continuum of healthcare. But there are actionable solutions we’ve outlined throughout this Horizon Report, let’s start with a clear view of where the vulnerabilities lie.
Breaches, 2023 vs 2024
Patient Records Exposed from 2022 - 2023
Business Associates continued to lead as the largest contributors to breaches, yet Health Clearing Houses saw an alarming 2453% year-over-year increase in exposed records. This sharp rise highlights the growing vulnerability of entities that manage massive volumes of sensitive patient data and critical healthcare services.
Healthcare leaders need to prioritize securing these high-risk entities. Strengthening protections and ensuring compliance with evolving cybersecurity standards is no longer optional – it’s essential to mitigating risks and maintaining trust in the healthcare ecosystem.
Type of Entity Reporting a Breach, 2023 vs 2024

Business Associate
Person or organization that performs a function or activity on behalf of a covered entity but is not part of the covered entity’s workforce. Can also be a covered entity. BAs can be the source of the breach or part of it (“BA Present”).
Health Plan
Entity that assumes the risk of paying for medical treatments, e.g., uninsured patient, self-insured employer, payer, or Health Maintenance Organization (HMO).
Healthcare Clearing House
An institution that electronically transmits different types of medical claims data to insurance carriers, e.g., pharmacy claims, dental claims, inpatient and outpatient claims, etc.
Healthcare Provider
A person trained and licensed to give health care; a place licensed to give health care, e.g., doctors, nurses, and hospitals.
Health Clearing Houses saw an alarming 2453% year-over-year increase in exposed records.
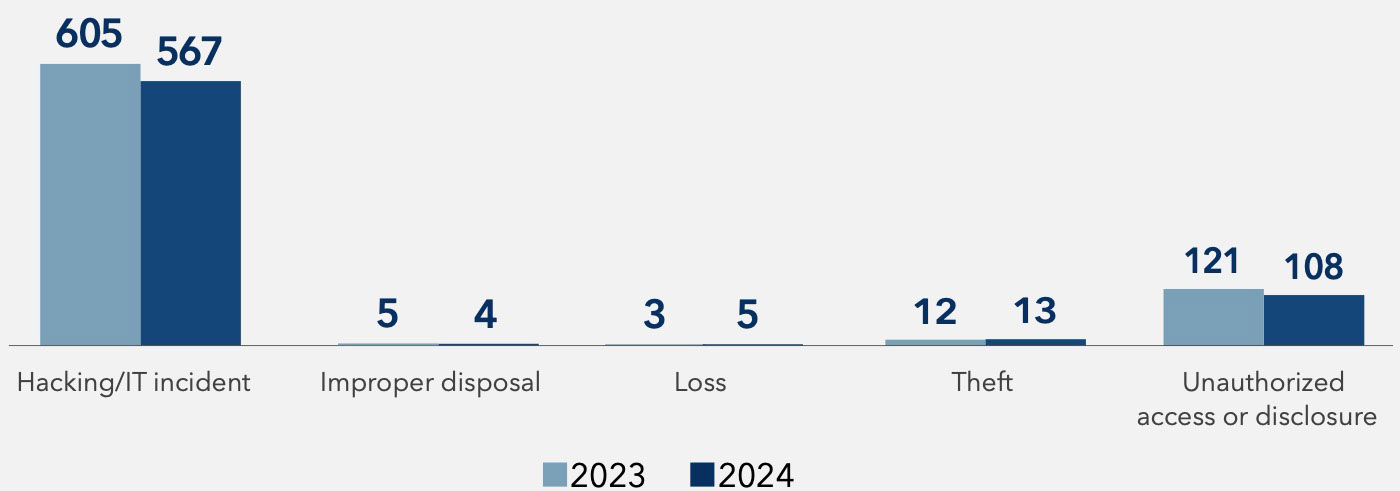
Hacking and IT incidents accounted for 91% of all breaches in 2024, cementing their status as the most devastating and impactful cybersecurity threat to healthcare. These attacks weren’t just frequent—they were sophisticated, targeting healthcare’s most critical systems with precision and intent.
Ransomware attacks led the charge, crippling organizations by locking down essential systems and demanding exorbitant payouts. Recovery costs often far exceed ransom demands, with downtime creating chaos for care delivery, delaying treatments, and straining operations.
Malware and spyware attacks designed to siphon information over time or disrupt operations outright infiltrated network servers and endpoints. These stealthy intrusions are often undetected for months, amplifying their impact and creating cascading risks. The stakes couldn’t be higher. Hacking incidents continue to dominate the threat landscape, posing risks to patient safety, operational continuity, and healthcare trust.
Type of Breaches, 2023 vs 2024
Hacking/IT Incident
Includes malware attacks, ransomware, phishing, spyware, or unauthorized card fraud.
Theft
Unauthorized removal of information from a system without the owner’s knowledge or authorization.
Improper Disposal
Misplaced or improperly decommissioned devices and files.
Unauthorized Access/Disclosure
When a patient’s Protected Health Information (PHI) is accessed by a third party without legal authority.
Loss
Accidental misplacement of equipment or storage containing patient records.
In 2024, attackers leaned into familiar vulnerabilities while testing new threat vectors. Email breaches rose by 18%, reinforcing phishing as a go-to tactic.
Laptops aren’t just tools; they’re targets. 2024 saw a 125% spike in breaches, highlighting the risks tied to portable devices in modern healthcare. Stronger encryption and better endpoint management can turn this weak link into a line of defense.
Location of Breach Information, 2023 vs 2024
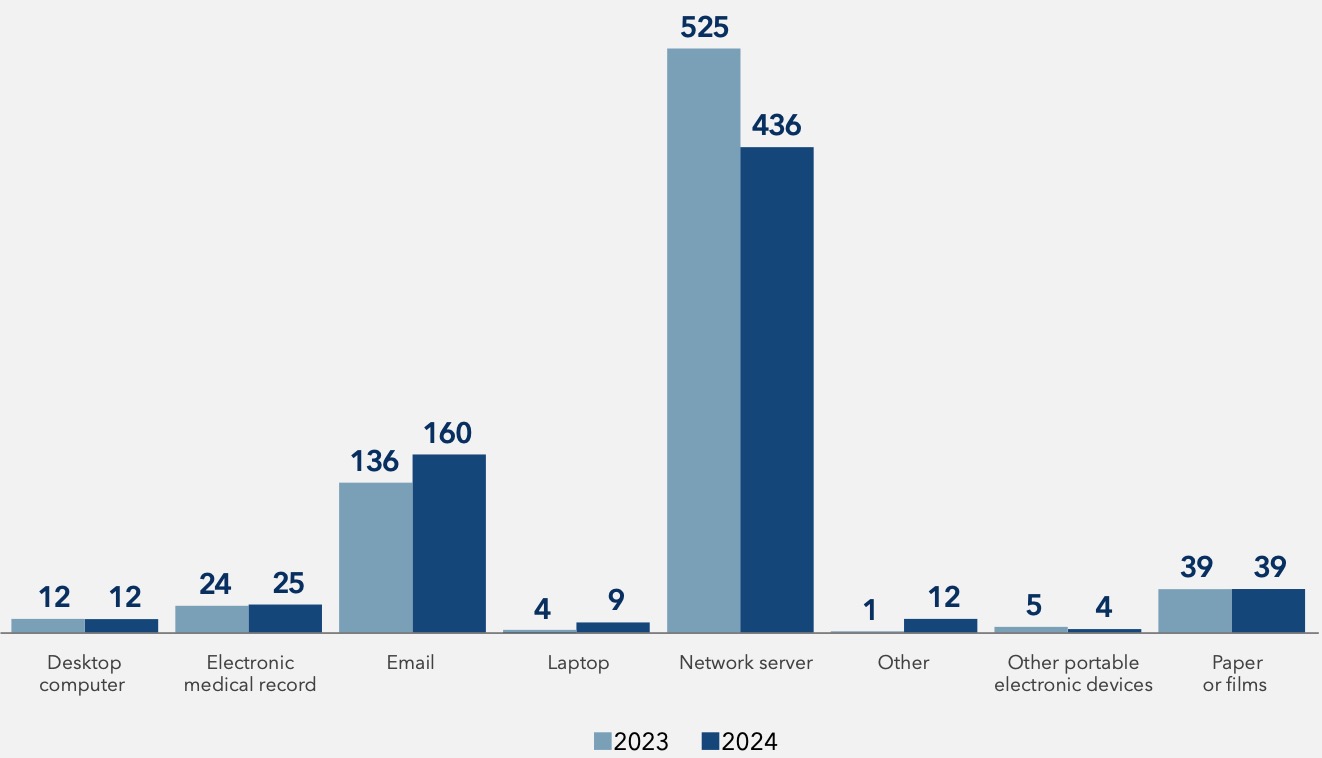
125% spike in laptop breaches in 2024
The 2024 data reveals a dual challenge for healthcare organizations: managing third-party risks and addressing vulnerabilities within their walls. Business Associates remain a significant source of breaches, while Health Plans and Clearing Houses underscore the risks inherent in interconnected systems. These third-party dependencies amplify the need for robust vendor management, compliance oversight, and collaborative risk mitigation strategies.
With breaches rising significantly in 2024, healthcare providers’ email and portable devices have emerged as critical weak points. Phishing attacks and poor endpoint security remind us that even familiar tools can become liabilities without adequate safeguards. These internal vulnerabilities demand focused efforts to strengthen defenses, train staff, and adopt advanced security measures.
Protecting patient data in 2025 requires a holistic approach that addresses internal risks and third- party threats.
It all starts with empowering healthcare leaders to build a resilient, secure future for their organizations and patients.
This report is based on data collected from OCR’s databases and public records, covering the periods from January 1, 2023, to December 31, 2024. We have undertaken efforts to scrub and clean the data to remove duplicates, ensuring higher accuracy and reliability. While we strive to maintain the integrity and accuracy of this data, please be aware that data content and accuracy may change over time due to periodic updates and additions by the OCR. Fortified disclaims any liability for errors or omissions in this data.
For further details or questions, please contact our team at connect@fortifiedhealthsecurity.com.
Healthcare organizations face a critical challenge: securing patient data while navigating tight budgets and a growing cybersecurity workforce shortage. With the looming cybersecurity workforce shortage expected to reach 85 million professionals globally in the next five years, healthcare systems are under increasing pressure to maintain strong defenses with limited resources.
In 2024, healthcare data breaches affected over 165 million individuals, highlighting the urgent need for stronger cybersecurity. Tight budgets make it harder to address these challenges, especially as new technologies like IoMT devices and AI platforms increase security risks. Despite these constraints, healthcare organizations can still prioritize cybersecurity and reduce risk while maximizing value.
As healthcare organizations adopt rapidly evolving technologies—such as EHRs, IoMT devices, and AI- driven tools—the need for regular security updates and maintenance increases. These investments are crucial for improving patient care, expanding the attack surface, and creating new cybersecurity challenges.
Projections show the IoMT market growing from $48.7 billion in 2022 to $370.9 billion by 2032, driving further demand for secure systems. However, with tight budgets, healthcare organizations must carefully prioritize these investments. Balancing the need for cutting-edge technology with the imperative to secure patient data requires smart, cost-effective strategies that maximize value while mitigating risk.

Global Internet of Medical Things Market (IoMT)
Organizations should conduct comprehensive risk assessments to identify critical assets and vulnerabilities and then assign resources to high-level risks. Not every element of your IT infrastructure requires the same level of security.
Focus on high-impact, low-cost cybersecurity solutions, embracing initiatives that offer the highest ROI. For instance, multifactor authentication (MFA) and phishing awareness reduce risk without significant investment.
Healthcare cybersecurity priorities should also emphasize medical device security since this directly affects patient care. Vulnerability management for IoMT mitigates device security risks.
Organizations also experience data breaches through third-party vendors. Third-party risk management programs rank vendors, allowing organizations to focus on their highest ranked vendors driving mitigation activities to reduce risk”.
Healthcare can also mitigate risk by aligning cybersecurity investments with regulatory compliance. They can protect patients, data, and devices while meeting HIPAA/HITRUST regulations, provide more value, and avoid fines and penalties.
Cybersecurity investments don’t have to be – and shouldn’t be – “one and done.”
Cybersecurity investments don’t have to be–and shouldn’t be–”one and done.” Organizations can first mitigate critical risks and phase in other investments over time.
Hospitals must identify cost-effective solutions along with areas where cutting costs is dangerous. Patient safety and data protection must come first; these are non- negotiable areas where cutting costs can lead to severe consequences.
Invest in HIPAA regulations training to ensure compliance and protect patient health information (PHI). Regular audits and ongoing staff education reduce human error, a leading cause of data breaches. A well-trained security team serves as a human firewall, preventing costly cyber incidents.
Layer encryption and access controls to safeguard patient data from unauthorized access. These measures protect sensitive information and minimize the impact of potential breaches.
Many organizations rely on multiple security vendors, leading to inefficiencies and high costs. Conduct regular assessments of vendor tools and contracts to identify redundancies and improve cost-effectiveness. Consolidation efforts can reduce expenses while maintaining or improving your security posture.
Improperly configured cloud solutions are a common source of security risks. Implement cloud security posture management to ensure compliance and protect cloud environments from threats.
Cyber insurance provides a financial safety net for managing the aftermath of cyber incidents. However, insurers require proof of robust security practices, such as deploying and operationalizing Extended Detection and Response (EDR) tools. Meeting these requirements ensures coverage and reduces financial risk.
Organizations can demonstrate the value of cyber investments in patient safety, compliance, and outcomes. HIPAA violations can lead to fines of up to $1.5 million per year for each violation category. Robust cybersecurity maintains compliance. An effective cybersecurity program costs less than fines from a single major HIPAA breach.
Let’s use this healthcare ROI formula. ROI = Financial gains / Improvement investment costs. A $100,000 cybersecurity investment can prevent up to $300,000 in breach-related costs— offering a 3x return on investment. Data Loss Prevention (DLP) solutions are an example of a low-cost investment that pays for itself many times over.
Organizations should also consider strengthening their cybersecurity posture to reduce cyber insurance premiums. If a robust cybersecurity program reduces insurance premiums by 15%, which is feasible, on a $1 million annual premium, that’s $150,000 in direct savings.
Value of Cyber Investments
$300,000
saved in breach-related costs
/
$100,000
cybersecurity investment
ROI = $3 in value for every $1 invested
In the face of a cybersecurity talent shortage and tight budgets, healthcare organizations can enhance their security posture through strategic partnerships. Collaborating with entities like H-ISAC, universities, and healthcare-specific MSSPs helps share resources, expertise, and threat intelligence.
This global, member-driven nonprofit allows organizations to share cyber threat intelligence, collaborate on best practices, and reduce costs through shared resources.
Partnering with this public-private initiative provides access to free, healthcare-specific cybersecurity resources that enhance security without exceeding budget.
Collaborations with universities help create training programs and internship opportunities, addressing the cybersecurity skills gap.
Working with technology vendors to develop customized security solutions ensures core clinical systems are protected without the need for extensive in-house expertise.
Outsourcing to MSSPs provides 24/7 monitoring, threat intelligence, and incident response, offering enterprise-grade security at a fraction of the cost of an in-house team.
Securing the future of healthcare requires prioritizing cybersecurity to protect patient care and data. By making smart investments in talent, technology, and strategic partnerships, healthcare organizations can strengthen their security posture without exceeding budget constraints. A clear ROI justifies each investment, ensuring that cybersecurity is not only an expense but a crucial component of patient care and regulatory compliance.

Guest Author
01
Cybersecurity threats to patient care and business operations, and their potential for significant financial, regulatory, and patient trust impacts.
02
The need to balance trust with the urgency to utilize AI and other technologies to drive innovation, quality, and efficiency.
03
Regulatory and stakeholder expectations for boards to actively oversee the management of cybersecurity and technology risks.
As a result, cybersecurity leaders are gaining greater access to their board. Being able to successfully engage to articulate risks, the strategy of their program, and the value it delivers can help a security leader build long term success.
A board wants to know four broad things –
Those are not yes or no questions, and a security leader can stimulate informative discussion by telling the story of their program. Keep the slides to a minimum and aim for a discussion on the factors that cause risk, how the program protects and enables business strategy, and the challenges faced.
Approach the discussion like a business plan and speak in terms of –
Focus on bringing solutions, not just problems. Cybersecurity is a big risk in healthcare, and your board knows that, so it is important to have an action plan or strategy for every risk raised.
Metrics add credibility to your story when used properly. They can show the effectiveness of the program by measuring coverage, speed, and accuracy. They can highlight efficiencies gained through automation, innovation, and productivity. Most importantly, metrics can support the story of reducing risk, preventing events, and returning value from investments. Unfortunately, metrics can also be a distraction, confusing, and overwhelming to a board, so it is important not to let them become the story.
Think of metrics like a pyramid. The dashboard a security leader uses to run and monitor day-to-day operations is the base – wide with deep details and measures. The messages and data used in discussions with business leaders are the middle – less detail and more combining of metrics to highlight operations and business impacts. What goes to the board should be the peak – less data and rolled up summaries that point to a story.
For example, cybersecurity SOC tools can produce metrics such as Mean Time to Detect (MTTD), Mean Time to Respond (MTTR), True Positives/False Positives, and the total number of security incidents detected. Those are important for running the security program but are not the right level for a board meeting. A summary of “Threat Detection & Response Capabilities” that is based on a roll-up of those metrics would be more relevant. Similar rolled-up measures can tell the story of other key risks such as third-party risk management, compliance, and cloud security posture.
One last note on metrics – be certain you can explain and prove the accuracy of anything you present to the board, and why it is relevant. A good rule of thumb for gauging relevancy is to ask, “what does it mean if this measure changes?” – if it doesn’t drive a response, it is likely not needed.
Be proactive about getting information to your board.
The chairman of the audit committee at my last company used to always ask me, “What is keeping you awake at night?” at the end of my quarterly updates. I realized the genius in that question was to give me a chance to break from PowerPoint slides to an open discussion. While meeting times with a board tend to be tightly scheduled, engaging in discussion makes for an effective meeting. Some practices to facilitate discussion include:
A strong board wants to understand the risks and how they are being addressed, so use every lever available to build their awareness.
Be proactive about getting information to your board.
Line up allies like the CIO, your Internal Audit leader, and Legal Counsel and pre-brief them on your message and metrics to rehearse your presentation, get feedback, and anticipate questions. Ask them to play the role of harsh critics to get issues on the table before the board meeting.
Remember, it is not limited to a once-a-quarter interaction at the board meeting. Clear it with your CEO, but the discussion can continue between board meetings with follow-ups on questions, sharing news relating to discussions, or awareness materials.
By making the most of interactions with the board, cybersecurity leaders can develop their role as business leaders and position their program for long term success.
More than a year ago, the Department of Health and Human Services (HHS) announced its intention to update the HIPAA Security Rule to better protect our healthcare infrastructure against a growing wave of cyberattacks. Yet, in the months since, healthcare providers, plans, and their partners have been hit with 472 breaches, underscoring both the urgency to act and just how interconnected we truly are. Any attack — even one at a small, rural hospital — has the potential to impact the entire ecosystem, threatening the stability of larger networks and putting providers, patients, and communities at risk.
In response, various legislative proposals have emerged with New York taking the boldest step by enacting its own stringent cybersecurity rules in a move that is likely to inspire other states to follow suit — especially if federal efforts remain stalled.
As additional states consider similar mandates, healthcare providers may soon find themselves navigating a complex landscape of overlapping federal and state requirements. Certainly, this could result in stronger sector-wide defenses, but it could also create challenges for consistent compliance across jurisdictions.
Originally intended as best practices, these goals are likely to become benchmarks that all healthcare providers must meet.
Any attack — even one at a small, rural hospital — has the potential to impact the entire ecosystem.
Three bipartisan legislative proposals were introduced in 2024, highlighting the urgency among policymakers to establish more rigorous standards, enhance accountability, and mitigate the growing cyber threats facing our nation’s healthcare systems.
Introduced in November 2024 by Senator Cassidy (R-LA), along with Senators Warner (D-VA), Cornyn (R-TX), and Hassan (D-NH), this legislation focuses on improving the overall cybersecurity posture of healthcare and public health sectors through collaboration between the Department of Health and Human Services (HHS) and the Cybersecurity and Infrastructure Security Agency (CISA). It emphasizes the creation of a comprehensive cybersecurity incident response plan, offers grants for public or non-profit healthcare providers, and updates existing regulations to create cybersecurity standards. It also includes provisions for sharing threat information, enhancing training, and strengthening infrastructure. With Senator Cassidy currently serving as the ranking member of the HELP committee, and soon to become the Chair of that committee, we are hopeful that this bi-partisan legislation will pass early in the coming year.
Introduced in the Senate, then similarly in the House, the Healthcare Cybersecurity Act aligns with the Biden administration’s 2023 National Cybersecurity Strategy, emphasizing public-private collaboration and sector-specific security improvements. Building on this foundation, the act proposes enhancing resource allocation, establishing secure channels for real-time information sharing, and strengthening support for healthcare providers. The majority of items called out in this Act are items that are already being accomplished by CISA and HHS, but this legislation would solidify the future of these programs.
Proposed in the Senate, the Health Infrastructure Security and Accountability Act would mandate annual audits of large healthcare organizations, expand penalties for non-compliance, and, notably, require CEOs and Chief Information Security Officers (CISOs) to attest to their organizations’ cybersecurity compliance personally.
Additionally, the proposed bill allocates $1.3 billion in funding for critical access hospitals starting in 2027 to support resource-limited organizations. However, with phased penalties for non-compliance by 2028, many under-resourced providers may still face funding gaps.
While federal regulations remain stalled, New York’s proactive stance points to an obvious conclusion: What once was voluntary will soon be mandatory. Effective October 2, 2024, New York’s cybersecurity law requires hospitals to report cyber incidents within 72 hours and fully comply with extensive security measures within a year. Covering more than 200 hospitals, this mandate is the first of its kind in the U.S. and likely to set the stage for similar legislation at the state level.
As more states consider their own cybersecurity requirements, healthcare providers operating across state lines could face a layered mix of compliance obligations, navigating both federal and state-specific rules.
In July 2024, the public comment period closed for the Notice of Proposed Rulemaking (NPRM) under the Cyber Incident Reporting for Critical Infrastructure Act of 2022 (CIRCIA). This legislation, once finalized, will establish mandatory reporting rules across all critical infrastructure, requiring organizations to report cyber incidents within 72 hours and ransom payments within 24 hours.
The Cybersecurity and Infrastructure Security Agency (CISA) is currently reviewing the feedback received and aims to issue the final rule by October 2025. This impending regulation is designed to improve national response and resilience to cybersecurity threats by standardizing reporting protocols for significant incidents.
Given the potential impact on critical infrastructure, it is crucial for organizations to stay informed and prepare for compliance. We are closely monitoring the developments related to CIRCIA and recommend that our clients do the same to ensure readiness for these new reporting obligations.
As healthcare cybersecurity regulations evolve, leaders across the sector must act decisively. Building strong cybersecurity practices is no longer just about checking a box for compliance; it’s essential for safeguarding the healthcare ecosystem.
To effectively prepare for evolving requirements, healthcare providers should:
Providers should begin with a thorough assessment of their current cybersecurity landscape. Identifying and prioritizing gaps enables efficient resource allocation and targeted remediation.
While not all organizations may qualify, certain federal programs, including HHS’s proposed 2025 budget, aim to support under-resourced hospitals in implementing and maintaining essential cybersecurity measures.
As standards expand to cover non-PHI data, healthcare providers must ensure vendor contracts reflect updated security requirements. Regular assessments are crucial for verifying compliance, particularly as third-party vulnerabilities can become entry points for cyber threats.
Healthcare organizations without established cybersecurity programs must begin by tackling the essential goals. Meanwhile, those that already meet foundational standards would be wise to advance toward enhanced goals in anticipation of a future in which these benchmarks are the norm.
While new legislation will challenge all organizations, small and rural healthcare providers will face the greatest challenges. Despite initiatives from companies like Google and Microsoft offering discounted or free tools, adoption remains limited due to:
Many smaller providers rely on systems that may not integrate well with newer cybersecurity tools.
Organizations are cautious about how Google and Microsoft might handle their data, raising privacy and security concerns.
Limited budgets and a shortage of specialized cybersecurity talent prevent smaller providers from fully implementing these solutions, as well as monitoring and maintaining them.
Addressing these unique needs with adaptable, cost-effective solutions is a must — not only for their security but for the resilience of the entire healthcare system.
The shift toward mandatory cybersecurity standards reflects a critical, shared responsibility across the healthcare sector. Every organization—from large, multi-state systems to small rural providers—plays a critical role in preventing cyberattacks that create patient safety issues, and long-term patient confidentiality concerns.
Building a secure healthcare ecosystem is more than compliance; it’s about creating a unified system that protects patients, providers, and communities nationwide. Through public-private partnerships and real collaboration, healthcare leaders have an unprecedented opportunity to create a more secure future for everyone, but it will take all of us to make it a reality.
While AI offers unprecedented benefits to healthcare organizations, this technology is a double-edged sword.
As the healthcare ecosystem embraces the digital transformation artificial intelligence (AI) has provided – enhancing patient care, optimizing operations, and driving data-based decisions – it also creates new vulnerabilities that can endanger patient safety and disrupt hospital operations.
With the surge of Generative AI, cyber-attacks are becoming increasingly complex, forcing healthcare providers to balance finding ways to protect sensitive data and systems while innovating. But how can organizations do both? Let’s look at the evolution of AI-driven cyber-attacks, explore AI’s dual role as defender and disruptor, and identify the best strategies to build resilient healthcare systems with a balance of innovation and security.
AI-driven cyber-attacks represent a new class of threat vectors in which adversaries leverage machine learning and artificial intelligence to execute increasingly sophisticated attacks. These include everything from data breaches and disinformation campaigns to automated bot attacks and AI-generated phishing scams.
Generative AI’s malicious use makes it easier for cybercriminals to create more realistic, harder-to-detect, and more specific phishing attacks.
By training AI models on large text datasets to create emails that resemble a hospital’s official communication style or even the writing style of specific individuals, attackers are creating personalized messages that employees have more difficulty identifying as fraudulent.
Even the most well-trained healthcare staff can fall for these realistic phishing emails, and with hundreds or thousands of them inundating healthcare every day, it is not surprising to see the resulting stolen login credentials and compromised sensitive data.
According to trends we’ve witnessed with our customers, cybercriminals have shifted to employing AI to orchestrate complex attacks on one of their prime targets-hospitals.
AI-generated cyberattacks walk through every machine learning algorithm to find vulnerabilities within hospital networks so methods can be adjusted as needed. For instance, criminals can use AI to create ransomware that almost instantly learns how a hospital system works and intelligently shuts down its key services, making it impossible for that hospital to function without paying a ransom.
Healthcare data is among the most valuable information on the dark web, making AI- driven attacks on healthcare organizations especially harmful. Criminals can sell patient information for identity theft or manipulate records to disrupt care. The sophistication and adaptability of AI-driven attacks present a severe risk to patient privacy and data integrity, highlighting the urgent need for robust cybersecurity strategies in healthcare organizations. cybersecurity strategies in healthcare organizations.
Cyber-attacks are becoming increasingly complex, forcing healthcare providers to balance finding ways to protect sensitive data and systems while innovating.
We appear to be on a never-ending yo-yo in healthcare cybersecurity. While AI has been used in clinical settings for decades—primarily in decision support—it now plays a dual role, serving both attackers and defenders in cybersecurity.
For defenders, AI-powered tools are essential for identifying and responding to real-time threats. These systems can sift through mountains of data to identify abnormal behaviors that could be signs of a cyberattack, enabling the hospital cybersecurity team to take preventive action. Machine learning algorithms can even confirm vulnerabilities in a hospital network and propose ways to remain one step ahead of hackers.
Finding the right equilibrium between innovation and regulation is vital.
Al also plays a role in hospitals by analyzing data, predicting when beds might be available, and optimizing staff productivity overall. For example, Elon Musk suggested his new Al engine, Grok, can analyze medical images.
However, such applications bring particular cybersecurity risks. Because these systems rely on large volumes of patient data, a security breach could expose a significant amount of sensitive information. Also, if an Al system used in a diagnosis or treatment recommendation-perhaps through analyzing medical data on electronic health records-is manipulated, then it could lead to an inaccurate diagnosis or inappropriate treatment and directly affect patient care.
So, while the potential for diagnostics and health care is indeed fascinating, the risks are still being better understood.
From what we know today, addressing these risks demands a holistic approach:
Hospitals encrypt all patient information, making it only accessible to employees within the facility who are authorized to have it. Enhanced security measures, like two- step verification and restricted entry to specific AI programs, prevent the leakage of classified documents.
With a trusted partner like Fortified, healthcare providers receive expert-driven, continuous monitoring, ensuring they have the guidance and support needed to stay secure. Meanwhile, AI-driven monitoring systems complement these efforts by detecting real-time anomalies and alerting providers to unusual activity before it can escalate into a breach. Hospitals need comprehensive monitoring solutions that combine the expertise of a trusted partner with the power of advanced technology to identify and address emerging threats in real-time.
Audits, including “adversarial testing,” would identify and fix vulnerabilities in AI systems. While hospitals may not be able to launch a full-fledged red teaming effort, they can try penetration testing to get a feel for what type of attack their networks might see.
Human error remains one of the weakest links in security defenses, and hospital staff should be trained on cybersecurity dos and don’ts to reduce mistakes. Training staff in phishing strategies, methods of handling data securely, and password security can mitigate some risks.
Hospitals will benefit from the knowledge of other health organizations, security companies, and government partners, so cooperation with others is a must in managing AI and general cybersecurity risks.
Human error remains one of the weakest links in security defenses.
AI is transforming healthcare, offering huge potential for improving patient care and operations, but it also brings significant cybersecurity risks.
Healthcare organizations must adopt proactive and adaptable cybersecurity strategies to protect sensitive data and ensure patient safety. As AI technology continues to evolve, healthcare providers need to balance innovation with security, stay aware of emerging threats, and collaborate with regulatory bodies. By doing so, they can safely harness the power of AI while safeguarding their systems and fulfilling their mission of patient care.
Today’s attackers are more persistent and calculated than yesterday. They now employ an array of advanced tactics that demand a strategic and resilient cybersecurity posture from healthcare institutions. The anatomy of threat actor attacks in healthcare has become a sophisticated, multi-pronged threat, exploiting vulnerabilities across healthcare systems and data infrastructures.
So, how can healthcare organizations protect their data from these evolving threats? You must understand them. That understanding starts here with three new trends: the escalation of ransomware tactics, repeat attacks, and mega breaches.
Cybersecurity threats have evolved far beyond traditional ransomware. Known as “Ransomware 2.0,” double extortion tactics are now the norm. Attackers now not only encrypt the data but also steal it and threaten public release if the ransom is not paid. This raises the stakes, particularly for healthcare organizations, where patient confidentiality and regulatory compliance are crucial.
Today’s attackers are more persistent and calculated, employing an array of advanced tactics that demand a strategic and resilient cybersecurity posture from healthcare institutions.
Once doesn’t seem to be enough anymore for threat actors. Now they are increasing repeat attacks on healthcare systems, that are even more sophisticated than the first. For example, the 2023 & 2024 attacks on McLaren Health Care led to significant operational disruptions, with some patient services affected for weeks.
After an attack, healthcare providers may focus on restoring essential services, sometimes leaving longer-term security issues unaddressed. Attackers exploit these “post-attack gaps,” which might remain open while hospitals scramble to resume patient care.
Health systems often face “cyber fatigue,” where security teams are overwhelmed, making them more vulnerable to additional attacks. Even after an initial attack, healthcare organizations may struggle with follow-up defenses, especially if resources are stretched thin.
Cyber attacks are well known to affect the revenue operations of a facility. That impact is felt across the organization, including the security and IT departments. A loss in revenue makes needed investments exceedingly challenging.
Attackers now not only encrypt the data but also steal it and threaten public release if the ransom is not paid.
The scale and frequency of attacks have created a wave of mega breaches across the healthcare ecosystem, impacting millions of patients and generating significant regulatory and reputational fallout. With sensitive patient data and essential services at risk, healthcare cybersecurity leaders are under increasing pressure to respond effectively.
Recent examples include the Change Healthcare breach, the largest ever reported in the United States, which exposed 100 million patient records. This breach underlined the vulnerability of large data repositories and the widespread impact of these breaches.
To counter this, healthcare Chief Information Security Officers (CISOs) and IT leaders must prioritize creating a layered security strategy that goes beyond playing defense.
Healthcare systems need to create an integrated approach that includes:
Securing patient data and maintaining uninterrupted access to critical care services are paramount; there is no room for error. As a result, healthcare institutions are deploying layered security solutions that encompass preventive, detective, and corrective measures. These include advanced threat detection systems, network segmentation, frequent security assessments, and incident response simulations.
This layered, resilient security posture allows healthcare systems to stay one step ahead of sophisticated cyber threats. Do not misunderstand; these potential threats will never be eliminated, but a proactive, integrated approach to cybersecurity significantly reduces the risk and impact.
As healthcare cybersecurity continues to face intensified attacks from threat actors, healthcare organizations must strategically focus on resilience and proactive defense to face these evolving challenges. By building a layered approach, healthcare communities can build a stronger line of defense to better defend against sophisticated attacks. Embracing these principles will be crucial in adapting to a rapidly changing digital threat landscape and securing the future of healthcare.
Healthcare systems today are under constant pressure to protect patient data and maintain operations amid growing cyber threats. For leaders in healthcare, managing third-party relationships is key to ensuring security and resilience—yet these partnerships also bring significant risks.
Effective Third-Party Risk Management (TPRM) is key to identifying, assessing, and mitigating these risks. However, TPRM maturity varies widely across the industry. For healthcare leaders, advancing through TPRM maturity stages is essential to building a comprehensive risk management framework that protects patient trust, supports operational continuity, and strengthens organizational security.
Recent high-profile incidents underscore the significant risks healthcare organizations face due to third-party vulnerabilities:
July 2024
OneBlood, a major supplier of blood and blood products serving over 350 hospitals, experienced a ransomware attack that severely disrupted its blood delivery operations. This breach highlights the impact third-party disruptions can have on healthcare services, as well as the critical need to include essential suppliers in a comprehensive TPRM program
February 2024
Change Healthcare, a leading provider of services and solutions to healthcare organizations was targeted in the most significant HIPAA-regulated data breach involving protected health information (PHI). The ransomware attack compromised PHI for at least 100 million individuals, demonstrating the substantial risks posed when third-party vendors handle large volumes of sensitive data.
These cases demonstrate the critical need for a mature TPRM program to help proactively identify, evaluate, and mitigate third-party risks, ensuring operational continuity and safeguarding patient information.
Below are the five levels of TPRM maturity. Knowing your organization’s current level can help guide the targeted actions you should take to improve its security and resilience.
At the most basic level, many organizations lack a comprehensive and reliable inventory of their third-party suppliers. While critical partners, such as those providing EHR systems, patient accounting, or imaging services, may be informally identified, there is often no systematic record-keeping. Without a reliable inventory, effectively monitoring and managing associated risks is difficult.
Organizations at this stage should start by creating an accurate inventory of third-party suppliers and then conducting a BIA. A BIA identifies the most critical suppliers and assesses potential disruption impacts, setting the groundwork for progression to the next level.
At this maturity stage, organizations begin identifying critical third-party suppliers but do not completely understand the risks these suppliers pose to operational resilience.
Organizations must move beyond merely identifying critical suppliers and begin integrating them into a structured risk management process. This process includes
obtaining independent audit reports and reviewing control environments to establish a baseline for risk.
A mature TPRM program is essential to safeguard patient care and strengthen resilience against rising cyber threats. By advancing your TPRM maturity level and following the action steps outlined above, your organization can take a crucial step toward lasting security and operational stability.
By 2025, healthcare organizations will increasingly rely on managed security service providers (MSSPs) and specialized third-party vendors for cybersecurity. This strategy will help mitigate critical talent shortages, ease the burden on internal teams, and ensure access to advanced expertise and technology, enabling organizations to stay ahead of the rapidly evolving threat landscape.
In 2025, securing Internet of Medical Things (IoMT) devices will continue to pose significant challenges for healthcare organizations, with persistent vulnerabilities highlighted by a 2024 report from Forescout Research identifying medication dispensing systems as particularly exposed. Despite these challenges, healthcare organizations are increasingly prioritizing cybersecurity. A survey conducted between August and September 2024 revealed that 60% of health system executives plan to focus on improving cybersecurity in 2025.
However, the complexity of IoMT security, coupled with limited resources and competing priorities, means that comprehensive solutions may be slow to implement. As a result, while awareness and concern about IoMT vulnerabilities are rising, the pace of addressing these issues is tempered by the realities of the healthcare environment.
In 2025, the cost of cybersecurity insurance will rise as insurers respond to increasing breaches and ransomware attacks. Healthcare organizations without strong security measures will face higher premiums or be denied coverage, driving investment in robust cybersecurity. Those with mature defenses will secure better insurance terms, reduce breach risks, and enhance patient trust and care continuity.
Prediction: In 2024, states are expected to introduce enhanced cybersecurity regulations, following the rollout of key national and healthcare-specific strategies in 2023.

CEO, Fortified Health Security
As the CEO of Fortified Health Security, Dan Dodson brings over 17 years of experience leading healthcare and insurance organizations. Throughout his career, he has held pivotal leadership roles, including Executive Vice President at Santa Rosa Consulting, Global Healthcare Strategy Lead at Dell Services, and various leadership positions within Covenant Health System, The Parker Group, and Hooper Holmes. In 2018, Dan was recognized as a rising healthcare leader under 40 by Becker’s Hospital Review, and in 2022 he was elected to the Association for Executives in Healthcare Information Security (AEHIS) Board of Trustees. As a recognized thought leader in healthcare cybersecurity, Dan is a frequent speaker at industry events and conferences including CHIME, HIMSS, and HIT Summits.
Dan’s insights and data-driven expertise in cybersecurity, data privacy, risk management, and threat mitigation are regularly featured in popular media and trade publications such as Becker’s Hospital Review, Healthcare Business Today, and Healthcare Innovation News.

Independent Board Member, CISO
Paul has three decades in senior cybersecurity leadership roles at the White House, a big four public accounting firm, and a Fortune 100 company.
He built the first cybersecurity programs at the White House and HCA Healthcare and led them a combined 28 years in Chief Information Security Officer (CISO) roles. He also spent six years building a cybersecurity audit and consulting practice and became a partner at PricewaterhouseCoopers. Throughout, Paul has been a developer of leaders, with thirty-eight members of his teams selected for CISO positions.
Paul now focuses on raising the bar for CISO leadership. He is an independent director on the board of Fortified Health Security, technical advisor to the board of the U.S. Organ Procurement and Transplantation Network, and a developer of National Association of Corporate Directors programs. He advises and mentors CISOs as a faculty member at IANS Research; is an active cybersecurity and AI thought leader appearing in publications and conferences; and develops and teaches cybersecurity leadership programs at Belmont University.

Chief Information Security Officer, Fortified Health Security

Senior vCISO & Executive Director of Subsidy Program, Fortified Health Security
With over 30 years of experience in healthcare information technology, and over 13 years in healthcare cybersecurity, Kate Pierce has deep insight into the persistent challenge of improving security with increasingly limited resources. During her tenure as the CIO and CISO at a Critical Access Hospital, Kate spearheaded the creation of the organization’s security program, encompassing governance, strategic planning, and the selection and rollout of security controls. To further the cause of cybersecurity in healthcare, Kate actively collaborates with the HSCC CWG and the 405(d) program, and consistently advocates at the federal and state levels to fortify cybersecurity within healthcare organizations.

VP Advisory Services, Fortified Health Security
Jason Myers brings over 20 years of experience in healthcare, IT operations, and cybersecurity to Fortified. He previously served as Head of IT Central Services at Amazon and held leadership roles at MEDHOST, including Chief Information Officer.

vCISO, Fortified Health Security

Director of Cybersecurity Operations, Fortified Health Security
Fortified is Healthcare’s Cybersecurity Partner® – protecting patient data and risk throughout the healthcare ecosystem.
A managed security service provider that has been awarded many industry accolades, Fortified works alongside healthcare organizations to build customized programs designed to leverage their prior security investments and current processes while implementing new solutions that reduce risk and increase their security posture over time.
Led by a team of industry-recognized cyber experts, Fortified’s high touch engagements and client-specific process maximize engagement value and deliver an actionable, scalable approach to help reduce the risk of cyber events.